 Book Appointment
Book Appointment
Living with an anal fistula can be painful, embarrassing, and emotionally draining. Patients often hesitate to discuss their symptoms due to the sensitive nature of the problem, which can delay proper treatment. If you are experiencing persistent discharge, pain, or swelling near the anal region, you may be suffering from a Fistula-in-Ano. We specialize in the diagnosis and advanced surgical management of anal fistulas. With over 25 years of surgical expertise, more than 8,000 laparoscopic surgeries, and 400+ complex anorectal surgeries, we are committed to offering patient-first, minimally invasive, and highly effective treatments.
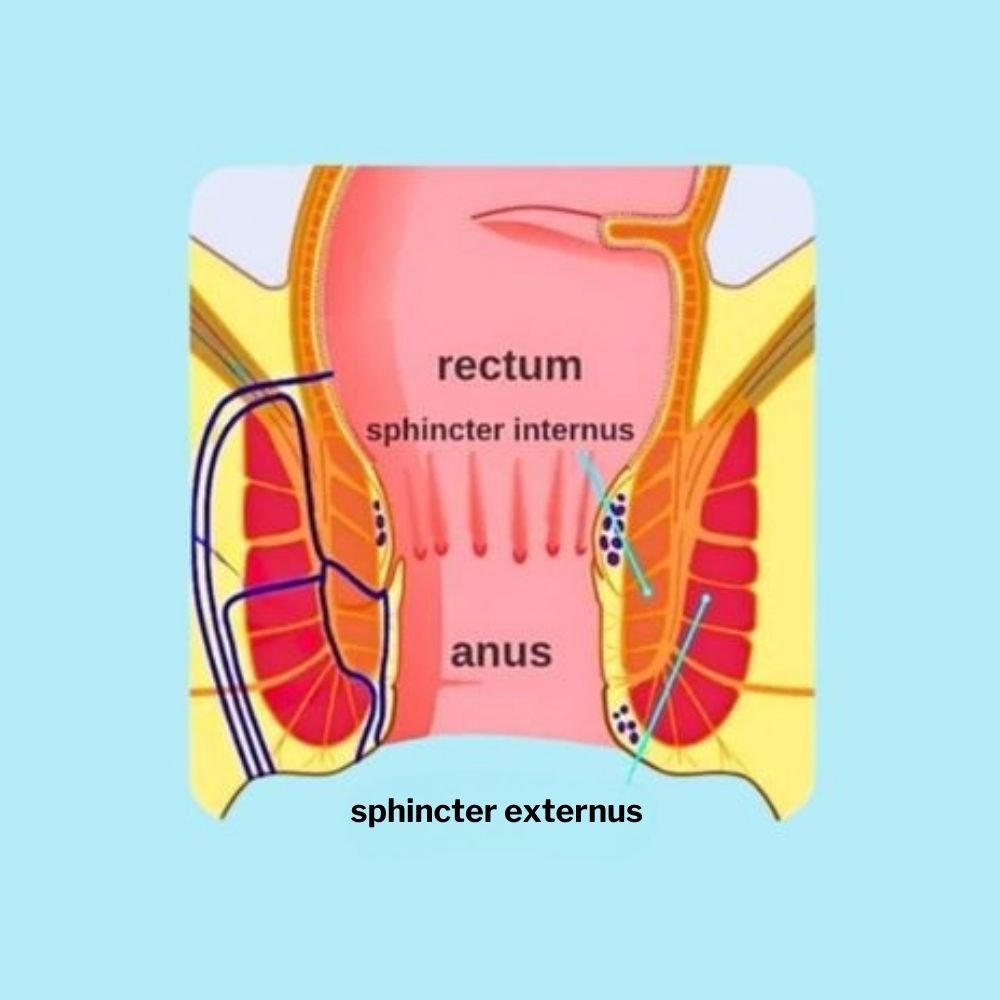
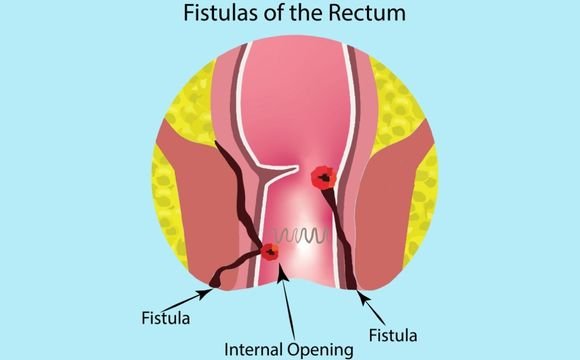
A Fistula-in-Ano is an abnormal tunnel-like tract that develops between the anal canal and the skin around the anus. It usually forms after an untreated anal abscess or chronic infection in the anal glands. It opens and connects the infected anal gland or the anal canal to a hole in the outer skin around the anus.
Since fistulas rarely heal on their own and often worsen over time, surgery is considered the gold standard treatment.
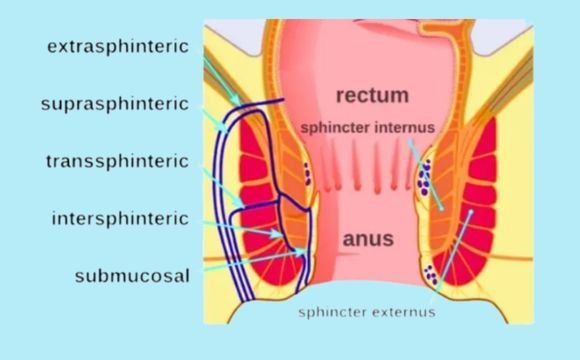
Understanding the type of fistula helps determine the best surgical approach.
Single tract, easy to treat.
Multiple tracts, often involving anal sphincter muscles.
Crossing sphincter muscles.
Higher tracts, more complex.
After previous unsuccessful surgeries.
A proper diagnosis ensures safe and successful surgery. At our center, we use:

You may be advised surgery if you:
Surgical procedures remain the most reliable and effective treatment for anal fistulas. Modern methods ensure faster recovery, less pain, and minimal complications.
From first consultation to complete recovery, here’s what to expect during the treatment journey.


While advanced techniques reduce risks significantly, patients should be aware of possible complications:
With 25+ years of surgical expertise, our complication rates are among the lowest.
| Surgery Type | Best For | Procedure Overview | Advantages | Limitations / Risks | Recovery Time |
|---|---|---|---|---|---|
| Fistulotomy | Simple, low fistulas not involving sphincter | Tract is cut open and allowed to heal naturally | High success rate, simple, cost-effective | Not suitable for high/complex fistulas; small risk of incontinence | 2–4 weeks |
| Seton Placement | Complex fistulas involving sphincter muscles | A surgical thread (seton) is placed to keep tract open, allowing gradual healing | Preserves sphincter, reduces risk of incontinence, good for staged treatment | May require multiple sittings, longer healing process | 4–8 weeks (with follow-ups) |
| LIFT Procedure | Transsphincteric / complex fistulas | Internal fistula opening is tied and closed while preserving sphincter muscles | Sphincter-sparing, low recurrence, less pain | Technically demanding, not suitable for all fistula types | 2–3 weeks |
| Advancement Flap Surgery | High or recurrent fistulas | Internal opening covered with a flap of healthy rectal tissue | Preserves continence, effective for difficult fistulas | Higher chance of recurrence compared to LIFT or laser | 3–4 weeks |
| Laser Fistula Surgery (FiLaC) | Simple and complex fistulas, minimally invasive option | Laser fiber is passed inside tract to seal it | Minimally invasive, less pain, faster healing, less bleeding, outpatient procedure | Slightly higher cost; long-term results still being studied | 1–2 weeks |
| Stapler / Ligasure-Assisted Surgery | Complex or high fistulas where precision is needed | Specialized stapling or energy device used to seal tract | High precision, reduced blood loss, faster healing | Not available everywhere; costlier | 2–3 weeks |
Patient Information Guide